
Markers that can effectively determine the extent of cerebrovascular aging are imperative, but more needs to be done. However, scientists have developed a set of white matter analysis techniques that can be used to estimate cerebrovascular age. This method can also be used to estimate brain nerve health and predict cardiovascular disease risk.
AI Analysis of white matter age of brain images from 1000 middle to old aged adults for predicting cardiovascular disease was published on Age & Aging
A research team comprising Dr. Huang Chu-Chung from the Department of Biomedical Imaging and Radiological Sciences of National Yang Ming Chiao Tung University, Distinguished Prof. Lin Ching-Po from the Institute of Neuroscience of National Yang Ming Chiao Tung University, and Dr. Chung Chih-Ping from the Department of Neurology of Taipei Veterans General Hospital used artificial intelligence algorithms to analyze the brain magnetic resonance imaging images of more than 1000 middle-aged and older adults. In their mathematical model, the volume of cerebral white matter can be used to estimate the physiological age of cerebral blood vessels. This information can serve as a basis for predicting cardiovascular disease. This research was published in Age and Aging, an influential journal in the field of aging research.
Prof. Lin explained that cerebral white matter deteriorates with age, and as it degenerates, it becomes diseased, resulting in cognitive impairment, dementia, and other diseases in older adults. Therefore, if the degree of brain nerve aging can be measured, potential cerebrovascular lesions and risks can be effectively identified.
Prof. Lin reported that a person’s age is not completely equivalent to their brain’s biological age because each person’s genes, diet, education, and living habits are different. This results in differential aging processes; two people of the same age may have different degrees of brain aging. Prof. Lin also reported that because cerebral neuropathy is most often associated with cerebrovascular diseases, people whose cerebrovascular age is higher than their actual age are usually at a higher risk of the diseases accompanying old age.
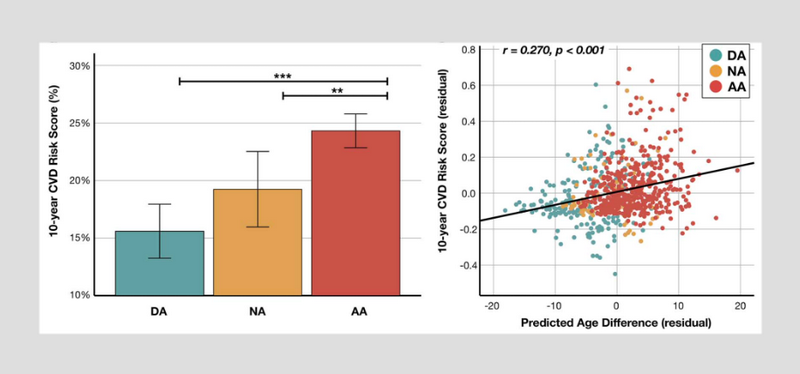
Prof. Lin’s research team also analyzed the risk of cardiovascular disease after 10 years by using the Flemingheim Cardiovascular Disease Risk Assessment System, which has been applied in various countries. Prof. Lin reported in the study that the risk of developing cardiovascular disease in the following 10 years is 5% higher in older adults whose white matter the age is higher than their actual age. However, Prof. Lin specified that the inferences of his study were based on a healthy population. For populations with cardiovascular disease or a risk of hypertension, hyperglycemia, and hyperlipidemia, further model correction and evaluation may be required. He added that the trained artificial intelligence models are relatively new, and longer-term geriatric tracking data would lead to more accurate inferences in the future.
The incidence and severity of cerebral white matter hyperintensity are proportional to a person’s age
Dr. Chung reported that cerebral white matter hyperintensity is the most common symptom of cerebral small vessel disease, responsible for 30% of strokes and 45% of dementia cases in the older population. In addition, the incidence and severity of cerebral white matter hyperintensity are proportional to a person’s age. However, in clinical practice, clinicians lack a standard of objective clinical assessment criteria independent of actual age.
Making objective clinical judgments regarding white matter lesion severity and future prognoses is difficult for middle-aged and older adults who have not yet developed apparent symptoms. Dr. Chung reported that the study could assist in understanding the correlation between cerebrovascular physiological age and cognitive function and reveal the associations between cardiovascular risk indicators —such as diastolic blood pressure, systolic blood pressure, and pulse pressure— and glycated hemoglobin. In addition to enabling the effective prediction of the risk of cardiovascular disease and mental deterioration associated with cerebrovascular aging, the study results have clinical value in that they can be used in predicting cerebrovascular physiological age.
A more effective evaluation treatment for aging diseases
In previous estimations of brain aging and brain age, Prof. Lin reported that brain volume was used to assess brain tissue atrophy and related cognitive deterioration. However, assessments of cerebrovascular disease risk were lacking. Prof. Lin believes that his research team’s breakthrough findings can be applied to more than simple assessments of people’s cerebrovascular health. For Taiwan, which is moving toward a super-aged society, the research findings can be used to assess the risk of cardiovascular disease in Taiwanese individuals or applied in clinical practice to evaluate the effectiveness of treatment for aging diseases.
